“For a long time, I witnessed a time when access to treatment was insufficient for many, leading to countless deaths. This motivated me to join the fight for better access to treatment,” says Alma de Leon, head of the International Treatment Preparedness Coalition—Latin America and the Caribbean
Treatment regimens in Guatemala were once complex and inaccessible to many people. Alma de Leon, head of the International Treatment Preparedness Coalition—Latin America and the Caribbean (ITPC-LATCA) and an activist for more than 20 years, says: “For a long time, I witnessed a time when access to treatment was insufficient for many, leading to countless deaths. This motivated me to join the fight for better access to treatment.”
Guatemala has since made considerable progress. In 2022, 95% of people living with HIV in Guatemala knew their HIV status, and 93% of people on treatment were virally suppressed. This was achieved through a combination of efforts, including streamlining HIV treatment regimens, introduction of dolutegravir, price reductions of dolutegravir, and closer collaborations between civil society, communities and the Government.
Alma says her proudest moment was when dolutegravir prices were reduced: “We fought for many years. We filed a lawsuit for dolutegravir access because it was very expensive—240 dollars. Eventually, after many years of struggle, we were included in a waiver, and dolutegravir was able to be procured for seven dollars.”
Before the reforms, there was a confusing system of more than 200 HIV treatment schemes. This has been reduced to fewer than 65 schemes. The health system refers people newly diagnosed with HIV to comprehensive care units, which seek to link them into treatment and care.
Multimonth dispensing of antiretroviral medicines has been introduced, which has been integral to improving adherence. Alma says: “People who have permanent jobs faced problems every month requesting permission to pick up their medicines during the day… people from rural, indigenous areas travel considerable distances to the health centres.”
Key gaps remain to be closed to keep the progress going. Data from 2023 show some reductions in progress towards the 95–95–95 targets, currently at 87–83–81. These may reflect larger factors affecting people living with HIV and people from key populations. For example, LGBTQI+ people in Guatemala face significant violence and discrimination.
Alma says more work needs to be done to facilitate “conducive environments” for people living with HIV: “It’s not just about having quality infrastructure. We need users of health services to feel comfortable and heard without prejudice. We need spaces of adequate sizes with drinking water, but we also need for staff in all health centres—from security guards to health professionals—to treat patients with respect and empathy. It is the time to recognize that behind every diagnosis, there is a human being who has shown resilience and the will to survive.”
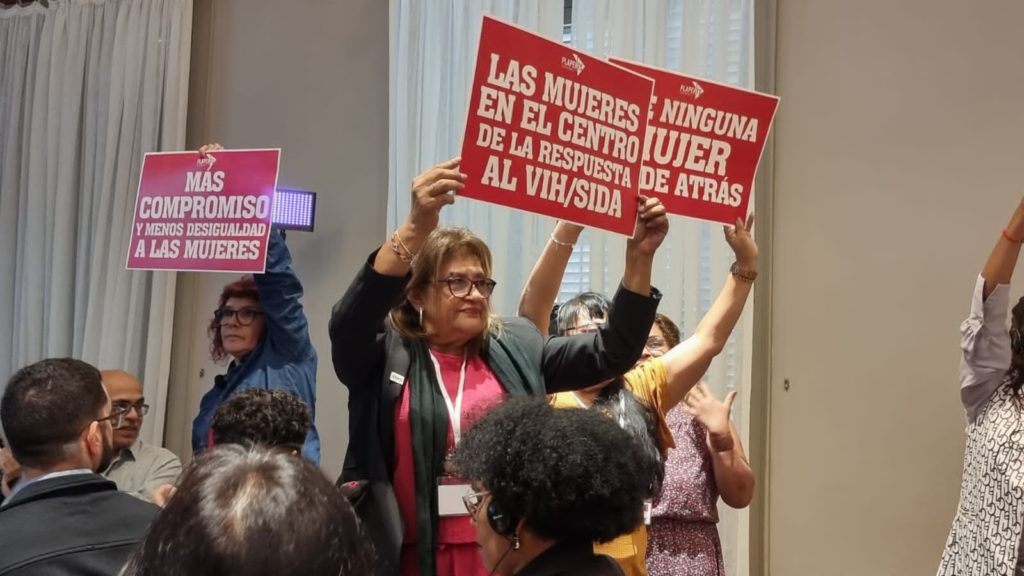
Community activism through ITPC-LATCA continues on this front. Alma says there are closer collaborations with the Government that bode well for reaching the 95–95–95 targets in the near future: “Our greatest achievement with the authorities is that we have moved from an activism of struggle and confrontation to an activism of dialogue at the decision-making tables.”